Table of Contents
Oral health is essential for a beautiful smile and is crucial in maintaining overall well-being.
Mounting evidence indicates that poor oral health and gum disease can have far-reaching effects on the body beyond the mouth.
This article explores the connections between oral health and various systemic health conditions supported by clinical studies.
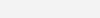
The Link Between Cardiovascular Disease and Poor Oral Health
Recent research has established a link between poor oral health and increased cardiovascular disease (CVD) risk.
Gum disease, specifically periodontitis, has been associated with inflammation and systemic bacterial dissemination, potentially contributing to CVD development.
A systematic review and meta-analysis published in the Journal of Clinical Periodontology found that periodontitis was associated with an increased risk of cardiovascular events (Chambrone et al., 2013).
Diabetes
The relationship between oral health and diabetes is bidirectional. Due to impaired immune responses, individuals with diabetes are more susceptible to gum disease, while periodontitis can adversely affect glycemic control.
A study published in Diabetes Care showed that treating gum disease led to improved glycemic control in individuals with diabetes (Engebretson et al., 2013).
Furthermore, a systematic review and meta-analysis published in The Lancet Diabetes & Endocrinology demonstrated that severe periodontitis is associated with a higher risk of developing type 2 diabetes (Simpson et al., 2015).
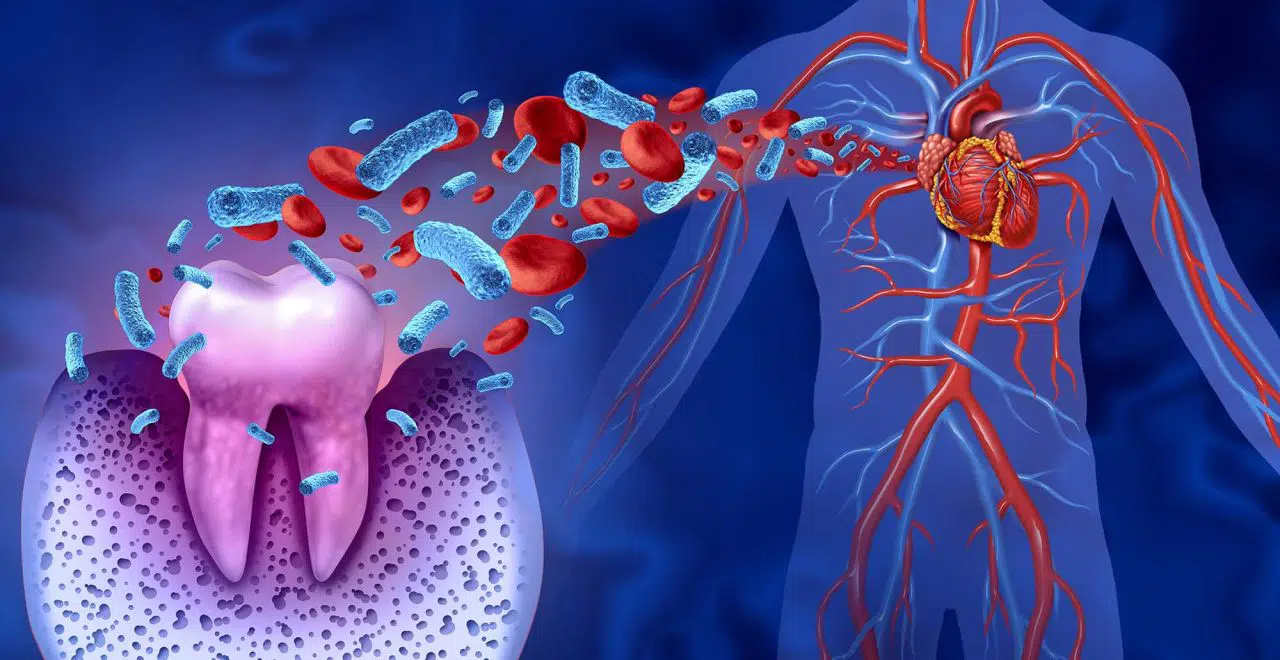
Respiratory Infections
Poor oral health has been linked to an increased risk of respiratory infections, including pneumonia.
Bacteria from the oral cavity can be aspirated into the lungs, leading to infection.
A study published in the Journal of Periodontology found that individuals with periodontal disease had a higher risk of developing pneumonia (Azarpazhooh et al., 2013).
Improved oral hygiene and regular dental care have been shown to reduce the risk of respiratory infections.
Pregnancy Complications
Oral health during pregnancy is crucial, as gum disease has been associated with adverse pregnancy outcomes.
Periodontal infections can trigger systemic inflammation, potentially leading to preterm birth and low birth weight.
A systematic review and meta-analysis published in the Journal of Periodontology indicated that treating gum disease during pregnancy reduced the risk of preterm birth (Ide et al., 2016).
Maintaining good oral hygiene and seeking dental care is vital for expectant mothers.
Hormones on oral health during pregnancy
The Impact of Oral Health on Cognitive Decline
Growing evidence suggests a potential association between poor oral health and cognitive decline, particularly in older adults.
Periodontal disease may contribute to the development of dementia and cognitive impairment.
A study published in the Journal of Alzheimer’s Disease found that individuals with periodontitis had a higher risk of cognitive decline (Kamer et al., 2015).
Maintaining optimal oral health may help preserve cognitive function. Good oral health and preventing gum disease are crucial for a healthy mouth and overall well-being.
Clinical studies have established strong connections between poor oral health and systemic health conditions, including cardiovascular disease, diabetes, respiratory infections, pregnancy complications, and cognitive decline.
Prioritizing oral hygiene practices and seeking regular dental care can protect one’s overall health and quality of life.
References
- Chambrone, L., et al. (2013). Periodontitis and chronic kidney disease: a systematic review of the association of diseases and the effect of periodontal treatment on estimated glomerular filtration rate. Journal of Clinical Periodontology, 40(5), 443-456.
- Engebretson, S. P., et al. (2013). The effect of nonsurgical periodontal therapy on hemoglobin A1c levels in persons with type 2 diabetes
Health Disclaimer: This article is for informational purposes only and is not intended to replace professional medical or dental advice, diagnosis, or treatment. Always consult a qualified healthcare provider with any questions or concerns about your health.