Table of Contents
Dental Cavities, also known as Cavities or Tooth Decay, are a common dental problem that occurs when the bacteria in plaque produce acid that damages the outer layer of the tooth, called the enamel. Over time, the acid can cause a hole or cavity in the tooth, becoming more prominent and deeper if left untreated.
Tooth decay is typically caused by poor dental hygiene, such as not brushing or flossing regularly or consuming sugary or acidic foods and drinks. It can also be influenced by dry mouth, gum disease, and genetic factors.
8 Ways To Prevent Dental Cavities
Preventing tooth decay is crucial for maintaining good oral health. Here are some effective strategies for preventing dental cavities:
1) Maintain proper oral hygiene
Brush your teeth using fluoride at least twice daily. Use a soft-bristled toothbrush and brush all tooth surfaces, paying special attention to the gumline. Don’t forget to brush your tongue to remove bacteria. Additionally, floss daily to clean between teeth and remove plaque and food particles.
2) Limit sugary and acidic foods/drinks
Sugary and acidic foods and beverages contribute to tooth decay. Reduce consumption of sugary snacks, candies, sodas, and fruit juices. If you indulge in these treats, brush your teeth or rinse your mouth with water afterwards to minimise the exposure to sugar and acid.
3) Opt for a balanced diet
Maintain a diet rich in fruits, vegetables, whole grains, lean proteins, and dairy products. These foods provide essential nutrients for overall oral health and support strong teeth and gums.
4) Fluoride for tooth strength
Fluoride helps strengthen tooth enamel and makes teeth more resistant to decay. Use fluoride toothpaste and consider using fluoride mouthwash as part of your oral care routine. If your water supply is not fluoridated, talk to your dentist about fluoride supplements.
5) Dental sealants
Dental sealants are protective coatings applied to the chewing surfaces of teeth, usually the premolars and molars. They create a barrier that helps prevent plaque and bacteria from accumulating in the deep grooves and pits of the teeth.
6) Regular dental check-ups
Schedule regular dental check-ups and professional cleans. Dentists can detect early signs of tooth decay and provide necessary treatments. Professional cleanings help remove plaque and tartar buildup that cannot be effectively removed by regular brushing and flossing.
7) Fluoride treatments
Your dentist may sometimes recommend fluoride treatments, especially if you are at a higher risk of tooth decay. These treatments involve applying a higher fluoride concentration to your teeth to strengthen the enamel further.
8) Consider dental X-rays
Dental X-rays can reveal decay between teeth or under the gum line, which may not be visible during a visual examination. Regular X-rays help detect early signs of decay and allow for timely treatment.
Remember, prevention is key when it comes to tooth decay. Following these preventive measures and maintaining good oral hygiene habits can significantly reduce the risk of developing tooth decay and maintain a healthy smile. Don’t forget to consult your dentist regularly for personalised advice and treatment.
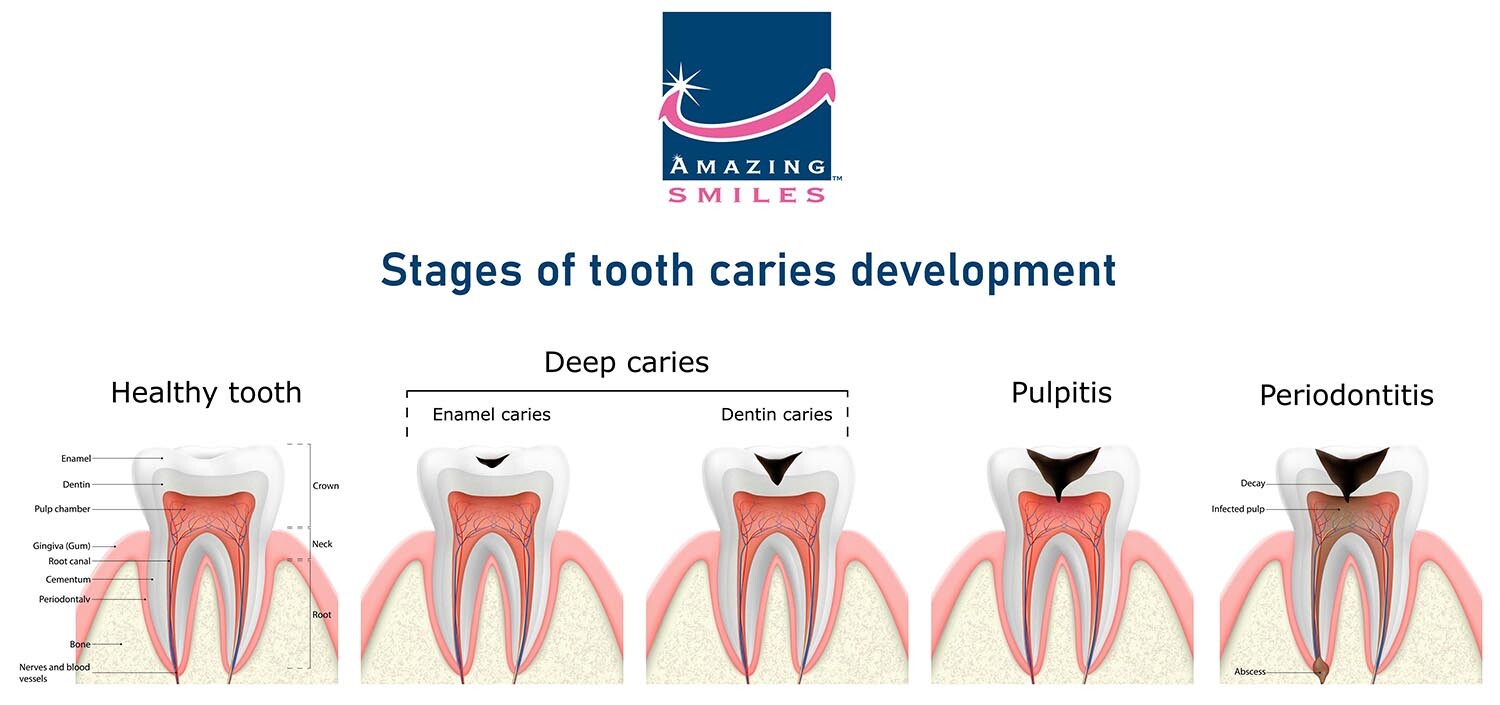
Stages of Dental Cavities/Tooth Caries
Tooth caries, commonly known as tooth decay or cavities, develops through several stages. Understanding these stages can help in the early detection and prevention of dental caries. It is essential to note that tooth decay is a progressive condition, and early detection and intervention are key to preventing further damage and preserving tooth structure. Here are the typical stages of tooth caries development:
Stage 1: Demineralisation and Enamel Caries
At this initial stage, acids produced by oral bacteria gradually demineralise the outer layer of the tooth, known as enamel. The enamel becomes porous, forming small white spots or chalky areas on the tooth surface. This stage is reversible with proper oral hygiene and professional dental intervention.
Stage 2: Enamel Breakdown and Dentin Caries
If left untreated, the demineralisation progresses, leading to enamel breakdown. Bacteria invade the underlying layer of the tooth called dentin, causing further decay. As dentin is softer than enamel, the decay spreads more rapidly. Symptoms may include tooth sensitivity, pain, or discolouration.
Stage 3: Pulpitis
Pulpitis occurs when the decay reaches the pulp, which contains blood vessels and nerves. The pulp becomes inflamed, causing moderate to severe toothache, increased sensitivity, and heightened pain. Root canal treatment may be necessary to remove the infected pulp and save the tooth.
Stage 4: Abscess Formation and Periodontitis
If tooth decay and infection progress untreated, an abscess may form at the tooth’s root. Abscesses are painful infections that can lead to swelling, facial pain, and the spread of infection to surrounding tissues. Advanced decay can also contribute to gum disease (periodontitis) and tooth loss. It is essential to note that tooth decay is a progressive condition, and early detection and intervention are key to preventing further damage and preserving tooth structure.
Symptoms of Dental Cavities
Symptoms of tooth decay can include tooth sensitivity, pain when chewing, visible pits or holes in the teeth, and discolouration or dark spots on the teeth. In its early stages, tooth decay may not cause noticeable symptoms, so regular dental check-ups and cleanings are essential to detect and treat tooth decay early. It’s important to note that there may be no noticeable symptoms in the early stages of tooth decay.
- Tooth sensitivity: Increased sensitivity to hot, cold, sweet, or acidic foods and beverages can be an early sign of tooth decay. When exposed to these stimuli, you may experience a brief, sharp pain or discomfort.
- Toothache: You may experience persistent or throbbing tooth pain as tooth decay progresses. The pain may be localised to a specific tooth or radiate to the surrounding area.
- Visible holes or pits: As decay advances, cavities or pits can form in the affected tooth. Depending on their size and location, these cavities may be visible to the naked eye or require dental X-rays for detection.
- Discolouration: Decayed areas of the tooth may appear brown, black, or white, contrasting with its natural colour. Discolouration can occur on the tooth’s surface or within the crevices and pits.
- Bad breath (halitosis): Tooth decay can contribute to persistent bad breath. Bacteria feeding on the decayed tooth produce foul-smelling gases, leading to an unpleasant breath odour.
- Unpleasant taste: If you notice a persistent unpleasant taste in your mouth, it could result from decayed teeth. Bacteria and decaying matter can leave a lingering, unpleasant taste.
- A sensation of a rough or broken tooth: Decay can cause the tooth surface to become rough or uneven. You may feel roughness or notice a broken or chipped appearance on the affected tooth.
- Gum inflammation: Advanced tooth decay can lead to gum inflammation and infection. This may result in red, swollen, or tender gums around the affected tooth.
Treatment for Tooth Decay
Treatment for tooth decay depends on the severity of the condition. In its early stages, tooth decay can often be treated with a filling, while more advanced cases may require a dental crown or root canal. Sometimes, the tooth may need to be extracted if it is severely decayed and cannot be saved.
- Dental fillings: Fillings are the most common treatment for cavities caused by tooth decay. After removing the decayed portion of the tooth, the dentist will fill the cavity with a dental material, such as composite resin, amalgam, or porcelain, to restore the tooth’s shape and function.
- Dental crowns: If the decay is extensive and has weakened the tooth structure, a dental crown may be recommended. A dental crown is a custom-made cap that covers the entire tooth, providing strength and protection. The decayed portion of the tooth is removed, and the crown is cemented onto the remaining healthy tooth structure.
- Root canal treatment: When tooth decay reaches the inner pulp chamber of the tooth, it can cause infection and severe pain. Root canal treatment may be necessary to remove the infected pulp, clean the root canals, and seal them to prevent further infection. After the root canal, a dental crown is often placed to restore the tooth’s strength and function.
- Dental bonding: Dental edge bonding is a procedure where a tooth-coloured resin material is applied and bonded to the tooth’s surface. It can repair minor tooth decay, chips, or cracks. The decayed portion is removed, and the resin is applied, shaped, and hardened with a special light, restoring the tooth’s appearance and function.
- Dental inlays and onlays: Inlays and onlays are indirect restorations used when tooth decay is too extensive for a filling but not severe enough to require a crown. Custom-made restorations fit into or onto the prepared tooth, providing strength and protection.
Extraction may be necessary in cases where tooth decay has severely damaged the tooth beyond repair. After extraction, the dentist may recommend tooth replacement options, such as dental implants, bridges, or dentures, to restore the missing tooth’s function and aesthetics.
Prevention is always better than treatment. Take control of your oral health and book a dental examination to assess the possibility of a dental cavity.
Our clinics across South East Queensland, including Gold Coast, Logan, Jimboomba, Bray Park, and Wynnum, are ready to provide comprehensive oral health care. As dental preferred providers, we offer selected services with no-gap fees, maximising the benefits of your private health coverage.