Table of Contents
Can Rheumatoid Arthritis Affect Your Teeth?
Rheumatoid arthritis (RA) is a chronic autoimmune disorder that primarily affects the joints but can also have implications for oral health, including the teeth.
Although the connection between RA and dental health may not seem evident initially, research has shown a significant link.
Below, we’ll explore how rheumatoid arthritis affects teeth and oral health.
Increased Risk of Periodontal Disease
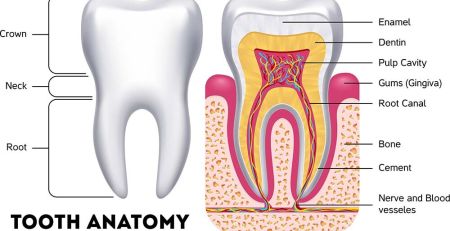
RA is associated with a higher risk of developing periodontal (gum) disease. In RA, the immune system mistakenly attacks the body’s tissues, leading to inflammation, including the gums.
Chronic inflammation can make it easier for bacteria to invade the gums, leading to gum disease.
Over time, gum disease can lead to the loss of bone that supports the teeth, resulting in loose teeth or even tooth loss.
Studies have shown that people with RA are up to twice as likely to develop periodontal disease compared to those without the condition.
Decreased Manual Dexterity
RA often affects the small joints in the hands, making daily oral hygiene challenging.
Stiffness, pain, and swelling in the hands and fingers can make it difficult to properly hold a toothbrush or floss.
As a result, oral hygiene practices may become less effective, increasing the risk of plaque buildup, dental cavities, and gum disease.
Dry Mouth (Xerostomia)
Many individuals with RA experience dry mouth, either due to the condition itself or as a side effect of medications.
Dry mouth, also known as xerostomia, occurs when the salivary glands do not produce enough saliva to keep the mouth moist.
Saliva protects teeth by neutralizing acids and washing away food particles.
The risk of cavities, gum disease, and oral infections increases without adequate saliva.
Can Rheumatoid Arthritis Medications Affect Your Teeth?

RA medications are crucial for managing symptoms and slowing the progression of the disease, but they can also have side effects that impact dental health.
Here are some ways that RA medications can affect your teeth and overall oral health:
Dry Mouth (Xerostomia)
Several medications commonly prescribed for RA, such as methotrexate and nonsteroidal anti-inflammatory drugs (NSAIDs), can cause dry mouth as a side effect.
A dry mouth reduces saliva flow, essential for neutralizing acids, remineralizing teeth, and reducing bacterial growth.
A lack of saliva can also increase the risk of tooth decay, gum disease, and oral infections. Without adequate saliva, the risk of cavities and gum disease increases, which can eventually lead to tooth loss.
Immune System Suppression
Disease-modifying antirheumatic drugs (DMARDs) and biologics, often used to manage RA, suppress the immune system to reduce inflammation.
However, this suppression can make individuals more susceptible to infections, including those in the mouth.
Gum infections can progress more rapidly in individuals on immune-suppressing medications, leading to more severe dental issues if not properly managed. Untreated gum disease can cause the supporting structures of the teeth, such as the bone and gums, to deteriorate, leading to tooth loss.
Gingival Overgrowth
Certain medications, such as corticosteroids, may contribute to changes in the gums, such as gingival overgrowth.
This condition can make it more difficult to clean the teeth properly, leading to an increased risk of plaque buildup, cavities, and periodontal disease.
Enlarged or inflamed gums are more challenging to clean effectively, increasing the risk of plaque buildup and periodontal disease, which can result in tooth loss if not properly managed.
How Do You Treat Tooth Pain Caused by RA?
Tooth pain in individuals with RA can result from various factors, including gum disease, joint inflammation, or medication side effects.
Here are some steps to manage tooth pain caused by RA:
Regular Dental Check-Ups

Seeing a dentist regularly is essential, especially if you have RA.
Regular dental cleanings and examinations can help catch dental issues early before they become more serious. Your dentist can also provide specific recommendations for managing RA-related oral health complications.
Manage Inflammation
Since RA is an inflammatory condition, controlling systemic inflammation is critical to managing oral discomfort.
Your rheumatologist may adjust your medication to control RA activity better.
Additionally, NSAIDs can reduce pain and inflammation affecting the jaw or other areas in the mouth.
Consult your healthcare provider before making any changes to your medication.
Maintain Good Oral Hygiene
Proper oral hygiene is crucial to prevent dental issues that can lead to pain.
Brush twice daily with a soft-bristled toothbrush, and floss once a day.
If manual dexterity is an issue, consider using electric toothbrushes or flossing aids for people with limited hand movement.
Antibacterial mouthwash may also help reduce gum inflammation and the risk of periodontal disease.
Keep the Mouth Moist
To alleviate dry mouth, drink plenty of water throughout the day and avoid beverages that can further dry the mouth, such as alcohol or caffeine.
Sugar-free chewing gum or lozenges can help stimulate saliva production.
Artificial saliva products are also available over the counter. They can help keep your mouth moist and reduce the risk of cavities.
Use Topical Treatments
Topical numbing gels or over-the-counter oral pain relievers may temporarily relieve tooth or gum pain.
Benzocaine products can be applied directly to the affected area for short-term relief.
However, these should be used as directed and with professional care.
Physical Therapy for the Jaw
If tooth pain is due to jaw joint issues, physical therapy exercises may help improve jaw function and reduce discomfort.
Applying warm compresses to the jaw can also relieve joint stiffness and pain.
Effects on Your Jaw from Rheumatoid Arthritis
Rheumatoid arthritis can significantly affect the temporomandibular joint (TMJ), which connects the lower jaw (mandible) to the skull.
RA affecting the jaw joint can lead to several issues:
Temporomandibular Joint Dysfunction (TMD)
RA can cause inflammation in the temporomandibular joint, leading to temporomandibular joint dysfunction (TMD).
Symptoms of TMD may include jaw pain, stiffness, limited range of motion, and a clicking or popping sound when opening or closing the mouth.
These symptoms can make it difficult to eat, speak, or perform everyday activities comfortably.
Jaw Stiffness and Limited Mobility
RA in the TMJ can cause joint stiffness, particularly in the morning or after periods of inactivity.
This stiffness may make it difficult to open the mouth thoroughly, complicating eating, speaking, and even oral hygiene tasks.
Over time, chronic inflammation can lead to permanent joint changes, reducing mobility.
Jaw Deformity and Bone Erosion
Severe, untreated RA can lead to bone erosion and joint damage, including the jaw joint.
Chronic inflammation can gradually wear down the bone in the TMJ, potentially causing changes in the jaw’s structure and alignment.
This can lead to an improper bite, facial asymmetry, and further complications in chewing or speaking.
Managing Jaw Issues Related to RA
- Medication Adjustments: Medications to reduce inflammation can help minimize TMJ involvement. Corticosteroids or DMARDs may be prescribed to address severe inflammation affecting the jaw.
- Jaw Exercises: Gentle exercises, often recommended by a physical therapist, can help improve jaw mobility and reduce stiffness. Stretching and movement exercises can prevent the joint from becoming too stiff and help maintain function.
- Orthotic Devices: Sometimes, your dentist may recommend a splint or mouthguard to help alleviate pressure on the jaw joint and reduce pain. This can be especially helpful if teeth grinding (bruxism) contributes to jaw discomfort.
- Cold and Warm Compresses: Cold packs can help reduce inflammation, while warm compresses may help ease muscle stiffness around the jaw. Alternating between cold and warm treatments can effectively manage pain and swelling.
Maintaining Oral Health While Managing Rheumatoid Arthritis
Rheumatoid arthritis is a systemic condition affecting the joints and various aspects of oral health, including the teeth and jaw.
RA increases the risk of periodontal disease, dry mouth, and complications involving the temporomandibular joint.
Medications used to treat RA, while effective for managing symptoms, can have side effects that impact oral health.
Proper management involves controlling inflammation, maintaining good oral hygiene, regular dental check-ups, and using tools and treatments to alleviate pain and improve jaw function.
By staying vigilant about RA management and oral health, individuals with RA can maintain better dental outcomes and reduce the condition’s impact on their overall quality of life.
Disclaimer: This article is for informational purposes only and should not be considered medical advice. Always consult your healthcare provider or dentist for personalized medical guidance regarding rheumatoid arthritis and oral health.