Gum disease, or periodontal disease, is a common condition affecting the gums and surrounding structures that support the teeth. Periodontitis progresses through various stages, each with symptoms and implications for oral health. Periodontal disease is a common dental health issue with significant consequences. To effectively control this condition, it’s crucial to identify it early, treat it appropriately, and continue with regular care.
This disease impacts the gums and the structures supporting the teeth. It originates from plaque accumulation on the teeth, a bacterial-laden sticky substance. If not cleaned adequately, this plaque turns into tartar, which results in gum swelling and infection.
What is periodontitis?
Periodontitis, or advanced gum disease, is a severe bacterial infection affecting the gums and surrounding structures. It occurs when bacteria accumulate on the teeth and gums, leading to inflammation and damage.
Untreated, Periodontitis can destroy the underlying bone and tissues supporting the teeth. However, with early intervention and diligent oral hygiene practices, the progression of periodontitis can be halted, preventing further damage to the bones and teeth.
Periodontal disease is a prevalent condition affecting approximately 10 per cent of the global population. It is characterised by an inflammatory response of the gums to plaque buildup.
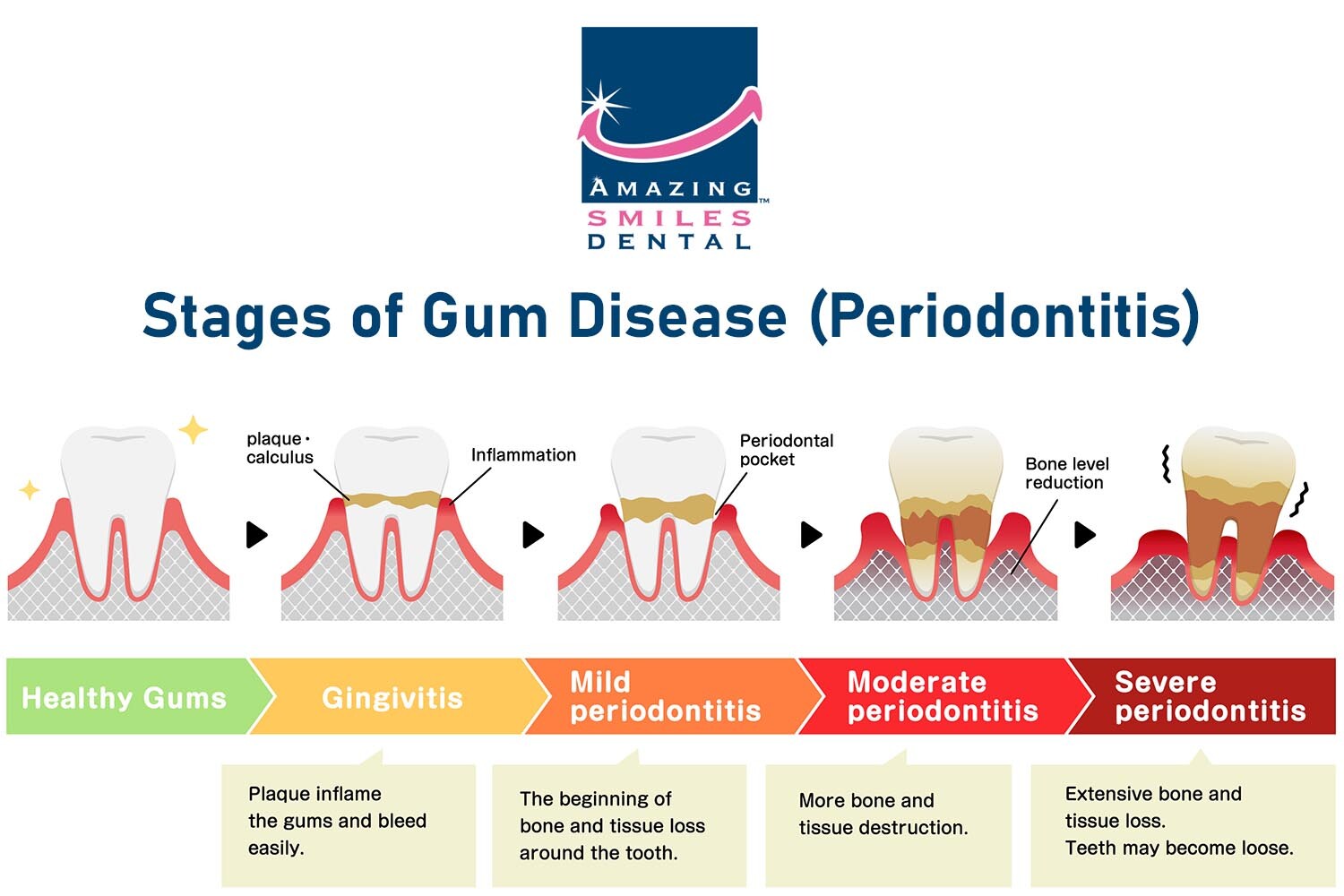
Stages of Periodontal Disease
Periodontitis initiates as gum inflammation and progressively worsens over time.
1. Stage One – Normal Tooth Health
At this stage, the gums are healthy, with no signs of inflammation or periodontal disease. Regular dental check-ups and good oral hygiene practices are vital for maintaining healthy gums and preventing the progression of gum disease.
2. Stage Two – Gingivitis
Gingivitis is the early stage of gum disease, characterised by inflammation of the gums. Common symptoms include redness, swelling, tenderness, and bleeding of the gums, especially during brushing or flossing. Gingivitis is primarily caused by poor oral hygiene, allowing plaque to accumulate and irritate the gum tissue.
Symptoms of periodontal disease include:
- Red, swollen, or tender gums
- Bleeding gums, especially during brushing or flossing
- Receding gums, making the teeth appear longer
- Persistent bad breath or a bad taste in the mouth
- Loose or shifting teeth
- Changes in the way your teeth fit together when biting
- Pus between the gums and teeth
- Formation of deep pockets between the gums and teeth
- Changes in the alignment of teeth
- Changes in the fit of dentures or other dental appliances.
3. Stage Three – Moderate Periodontitis
When left untreated, gingivitis can progress to moderate periodontitis. In this stage, the gum inflammation extends beneath the gumline, causing further damage. Symptoms may include persistent bad breath, receding gums, increased sensitivity, tooth mobility, and the formation of pockets between the gums and teeth. Plaque and tartar buildup and bacterial infection contribute to the progression of periodontitis.
4. Stage Four – Advanced Periodontitis
Advanced periodontitis is the most severe stage of gum disease. It involves extensive damage to the gums, connective tissues, and underlying bone structures. Symptoms may include severe gum recession, loose or shifting teeth, pus discharge, bad breath, bite changes, and eventual tooth loss. The infection can spread and affect an individual’s overall health and well-being.
Causes of Gum Disease?

The primary cause of periodontitis is plaque accumulation on the teeth and gums. Plaque is a sticky film composed of bacteria, food particles, and saliva.
When plaque is not adequately removed through regular brushing and flossing, it hardens into tartar or calculus, which cannot be eliminated through routine oral hygiene practices.
Tartar buildup provides a breeding ground for bacteria, leading to inflammation and infection of the gums. Other factors that can contribute to the development and progression of periodontitis include:
- Poor oral hygiene: Inadequate brushing and flossing allow plaque to build up, increasing the risk of gum disease.
- Smoking and tobacco use: Tobacco products impair the function of gum tissue cells and increase the likelihood of periodontal problems.
- Genetic predisposition: Some individuals may be genetically susceptible to gum disease, making them more prone to periodontitis.
- Hormonal changes: Hormonal fluctuations, such as those occurring during pregnancy or menopause, can make gums more sensitive to gum disease.
- Diabetes: Uncontrolled diabetes can affect the body’s ability to fight infection, increasing the risk of gum disease.
- Medications: Certain medications, such as oral contraceptives, anticonvulsants, and immunosuppressants, may affect gum health.
- Poor nutrition: A diet lacking essential nutrients can weaken the immune system and contribute to gum disease.
- Teeth grinding or clenching: Excessive force on the teeth and gums can damage the supporting tissues, making them more susceptible to infection.
- Certain systemic diseases: Conditions like cardiovascular disease, rheumatoid arthritis, and HIV/AIDS have been linked to an increased risk of gum disease.
- Stress: Chronic stress can impair the immune system’s response, making it harder for the body to fight off infections, including gum disease.
Risk Factors and Consequences of Untreated Gum Disease
Gum disease can lead to various complications and affect overall health. Risk factors include smoking, poor oral hygiene, hormonal changes, certain systemic conditions, genetic predisposition, and a weakened immune system.
Untreated gum disease has been associated with an increased risk of cardiovascular disease, respiratory infections, diabetes complications, pregnancy complications, and systemic inflammation.
How is Periodontitis Diagnosed?

Periodontitis is typically diagnosed through a comprehensive dental examination conducted by a dentist or periodontist. The diagnosis involves several steps to assess the health of the gums, teeth, and supporting structures. Here are the common diagnostic procedures used for periodontitis:
- Medical and Dental History: The dentist will review your medical history, including any previous oral health issues or treatments, and inquire about symptoms you may be experiencing.
- Visual Examination: The dentist will inspect your gums, looking for signs of inflammation, redness, swelling, and gum recession. They will also check for tartar buildup and any signs of infection or pus.
- Probing: The dentist will measure the depth of the spaces (periodontal pockets) between your gums and teeth using a dental instrument called a periodontal probe. Healthy gums typically have shallow pockets, while deeper pockets can indicate gum disease.
- X-rays: Dental X-rays may be taken to evaluate the bone levels supporting the teeth and detect any bone loss, a common sign of periodontitis.
- Periodontal Charting: The dentist may record detailed measurements of gum pockets and note any bleeding, recession, or other abnormalities in a periodontal chart. This helps track the progression of gum disease and guide treatment planning.
Based on the findings from these diagnostic procedures, the dentist can determine the presence and severity of periodontitis, classify it into different stages, and develop an appropriate treatment plan tailored to your specific needs.
It is important to remember that early detection and timely diagnosis of periodontitis are crucial for effective management and preventing further damage to the gums and supporting structures.
Periodontal Disease Treatment and Prevention

Prevention and early intervention are key to managing gum disease, and regular dental check-ups and proper oral hygiene practices are fundamental in preventing its progression. Treatment options for gum disease depend on the stage and severity. They may include scaling and root planing (deep cleaning), antimicrobial therapy, gum surgery, and regenerative procedures. For advanced cases, patients may be referred to a periodontal specialist for specialised treatment.
Gum disease progresses through various stages, from gingivitis to advanced periodontitis, with distinct symptoms and consequences. Seeking professional dental care from your nearest dentist is crucial in effectively treating gum disease and preserving oral health.
Why choose an Amazing Smiles Dentist near me?
At Amazing Smiles, we prioritise our patients’ convenience and strive to make dental care accessible to all. We are proud to accept all major private health funds, allowing our patients to maximise their dental benefits and make the most out of their insurance coverage. Moreover, we are dental-preferred providers, so we have established partnerships with specific health funds to offer exclusive benefits and affordable fees.
We understand that financial considerations may be a concern, and to ensure affordability, we provide flexible payment plans with no interest options. Our commitment to patient care extends beyond clinical excellence, as we aim to create a stress-free and comfortable experience for all individuals who trust us with their dental needs.